What is challenge?
Challenge is one of the elements by which an appraiser can add value to the appraisal discussion. It implies that the appraiser is actively contributing to the doctors’ thoughts on development and, by stimulating interest, may spur the doctor to more deeply explore their service delivery. Introducing challenge may allow a doctor to set goals, introduce learning into practice and encourage (further) development.
Setting an appropriate level of challenge, involves recognising where a doctor is in respect to an element of their practice and furthermore probing as to where they would like to be. At any given time in a doctor’s career they may need higher or lower levels of challenge. Some doctors will be self-driven (i.e. challenging themselves), whereas others may be “just doing the job” as they always have. The skilful appraiser will recognise the doctor’s engagement with challenge and can use the appraisal discussion appropriately.
An idea of what is being promoted in the concept of challenge is based on the demonstration of the ‘added value’ of the appraisal discussion. This “added value” is most often reflected in the right hand column of the appraisal summary (discussion and feedback).
Good preparation is essential to an effective appraisal discussion and this is clearly identified in the ADAM tool. A careful evaluation of the doctor’s evidence should lead to a list of appropriate questions. This gives the Appraiser the opportunity to introduce an appropriate level of challenge at the appraisal, hopefully leading to “added value”.
This concept involves ‘Evaluating the Evidence’ (EVE), both before and during the discussion.
Still missing from this equation is a means of ‘stratifying’ or assessing the level of development demonstrated by the doctor’s supporting information. For this purpose the “Taxonomy of Bloom” may be adopted/adapted.
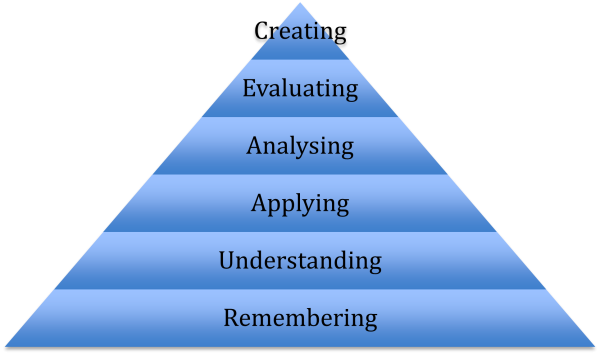
In the context of a medical appraisal discussion or evaluation of the evidence an entry may well, of course, demonstrate aspects of cognitive attainment at various levels in the hierarchy but to illustrate this in the context of the taxonomy simplified examples of evidence at each level are listed.
Remembering (Knowledge). A doctor has become aware (e.g. through reading) of new drugs to treat certain cancers, say, renal carcinoma or pancreatic cancers. That they exist, and that his patients may be prescribed these, constitutes new knowledge but the doctor may be entirely unaware of their mode of action or potential side effects.
Understanding (Comprehension). A doctor has attended a lecture on a new class of drugs (e.g. novel anticoagulants). She now understands the mode of action, indications, side effects etc. of these new drugs and sees the potential for prescribing these to her patient population. Experience of their use in practice is at this stage absent.
Applying. A doctor is quite familiar with prescribing a group of drugs, say Ace-inhibitors or Beta Blockers for hypertension etc. but following a useful medical meeting on the appropriate management of heart failure he is increasingly confident in using them in this context. He has taken the opportunity to review all his patients with this condition and ensured that their treatment was optimised whenever possible.
Analysing. A doctor has familiarised herself with recent arguments for and against PSA blood tests. She has modified her view of when to order this test in the context of the new learning and has now decided to obtain detailed informed consent from the patient before ordering it. She has greater confidence in discussing the pros and cons of this action and is prepared to discuss such issues more knowledgeably within the consultation.
Evaluating. A recent significant event within a GP practice team revealed that not all partners are managing a common medical condition in the same way. A meeting was called to discuss this and it was decided that at first the practice would run an audit on all patients diagnosed with the complaint in the last six months. A partner is assigned to look up current guidelines and to make recommendations to the group. A review meeting was arranged to study the audit data collection, to hear recommendations from the researching partner and to come to some consensus on management going forward.
Creating. A doctor made a diagnosis of Temporal Arteritis on clinical grounds in one of her patients. She was aware that there were clear guidelines regarding this on arranging a temporal artery biopsy but was dismayed to find that on ringing the local hospital there was no clear pathway on how this would be obtained. In consultation with the local consultant rheumatologist and the department of vascular surgery the doctor liaised to draw up new guidelines suitable for primary care services and arranged for these to be circulated to all practices within the health board area.
Feedback from experienced Appraisers would suggest that they naturally assess their doctors according to these stratifications but without being familiar with the hierarchy itself.
